A young woman who thought she had an eyelash in her eye shared her horror when she woke up three days later completely blind on the right side.
Rushed to the emergency room after having tests at her local opticians, Victoria Maddock, 27, was diagnosed with iridocorneal endothelial (ICE) syndrome – which is a swelling of the cornea, changes in the iris and glaucoma.
With glaucoma – where the optic nerve connecting the eye to the brain is damaged by a build-up of fluid in the front of the eye, increasing the pressure inside it – being most common in the over 70s, according to the NHS, Victoria was horrified.

“If I had left it even days later, I could have lost sight in my right eye completely due to the build-up of pressure – it doesn't even bear thinking about," Victoria said. “People think that glaucoma is an old person's disease, but I'm living proof that it can affect anyone at any age. I'm just so grateful that I didn't hold off any longer than I did to get it checked out by a specialist."

When Victoria's vision began to go blurry in her right eye, she thought it was because of a stray eyelash and bought some over the counter eye drops, hoping it would soon clear up.
But three days into using them, she woke up, opened her eyes and felt like she was “looking through milk bottle bottoms" and immediately rushed to the local opticians.
“For a few days my eye had been playing up and I thought nothing of it whatsoever. Then one day I woke up and I couldn't see out of my right eye at all, it was like a thick film had been placed over it," Victoria continued.
Victoria has worn prescription glasses for long distance since she was 18. She was soon told by experts that the pressure in her right eye was worryingly high. While normal eye pressure ranges from 18-22 millimeters of mercury (mmHg), Victoria's measured 28mmHg.
Opticians insisted that she went straight to hospital, where she was quickly diagnosed with ICE syndrome, caused by abnormal cells in the cornea migrating across the eye towards the iris, resulting in a build-up of pressure.

Not only is the condition rare – affecting 480, 000 people in the UK, but it is particularly unusual in her age group.
“By the end of the initial assessment I was surrounded by a group of doctors, all insisting on taking a look at my eye, as it was so unusual to see ICE in someone my age," Victoria explained. “It was pretty nerve-wracking. No one could believe I had glaucoma so young. One doctor said she'd only read about cases like mine before."

With her eye pressure reaching as high as 36mmHg, doctors booked Victoria in for a trabeculectomy on November 20, 2018 – a procedure to remove part of the iris, allowing fluid to drain more easily – for which she had a general anesthetic due to her “crippling fear of needles."
At first it seemed like the surgery had been a success, with Victoria taking two weeks off work for her eye to recover before she could expose it to natural light.
Relieved to have her sight back, she was given yet another blow three months later when she woke up to the same terrifying scenario.
“I was just getting my life back on track when I woke up with the same symptoms all over again," she explained. “I didn't waste a moment – going straight to the emergency eye care clinic. There doctors confirmed that the cells in my eye had begun to migrate back into my iris, effectively reversing the surgery."

Just a week later Victoria was back on the operating table in the same hospital, where surgeons repeated the procedure, but under a local anesthetic.
“Because I couldn't see out of the eye it wasn't half as bad I thought it would be, despite my needle phobia," she said.
Luckily, since the second operation, her eye has remained stable and now, determined to help others with the same condition, Victoria is working with eye research charity Fight for Sight to raise awareness of the prevalence of glaucoma, especially in younger people.

She is also campaigning for more people to realize the need to have regular eye tests – a minimum of once every two years.
“I never in a million years would have thought this could have happened to me," Victoria said. “I wear my glasses for watching TV and going to the cinema and that's about it. Now I've insisted all my friends and family get their eyes checked as soon as possible. It doesn't matter if you've got 20/20 vision, or if you're as blind as a bat – just go."
According to the Royal National Institute of Blind People (RNIB), glaucoma is so uncommon in young people that the Public Health Outcomes Framework indicator on avoidable sight loss due to glaucoma does not start counting people until they are over 40.
The RNIB's Specialist Lead for Eye Health, Dr. Louise Gow said, “usually glaucoma develops in older adults, typically with a close family history or from certain high risk groups such as African-Caribbean ethnic background."

“Although it's possible to develop primary open-angle glaucoma, the most common adult form of glaucoma, before the age of 40 – it is very rare," Dr. Gow continued.
For more information of Fight for Sight, visit www.fightforsight.org.uk



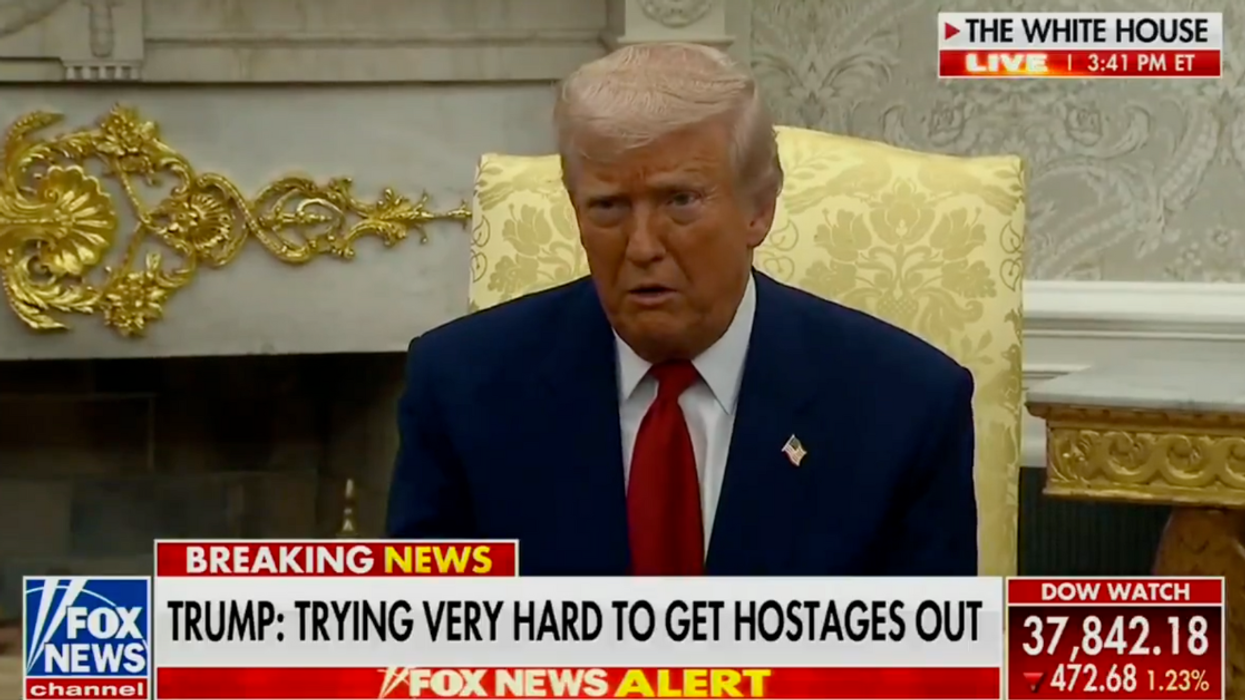



 @therealjeffreyross/Instagram
@therealjeffreyross/Instagram @therealjeffreyross/Instagram
@therealjeffreyross/Instagram @therealjeffreyross/Instagram
@therealjeffreyross/Instagram @therealjeffreyross/Instagram
@therealjeffreyross/Instagram @therealjeffreyross/Instagram
@therealjeffreyross/Instagram @therealjeffreyross/Instagram
@therealjeffreyross/Instagram @therealjeffreyross/Instagram
@therealjeffreyross/Instagram @therealjeffreyross/Instagram
@therealjeffreyross/Instagram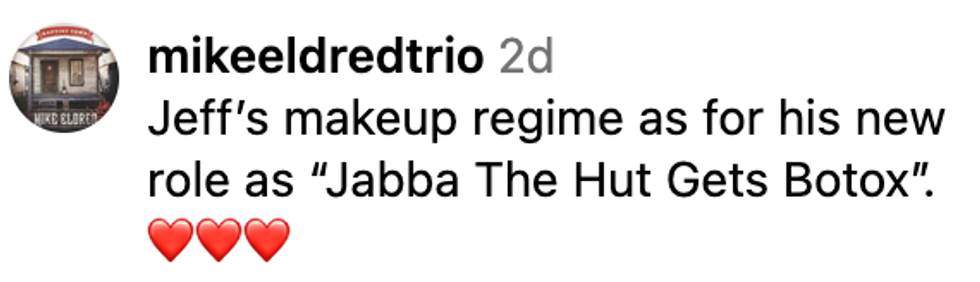 @therealjeffreyross/Instagram
@therealjeffreyross/Instagram @therealjeffreyross/Instagram
@therealjeffreyross/Instagram @therealjeffreyross/Instagram
@therealjeffreyross/Instagram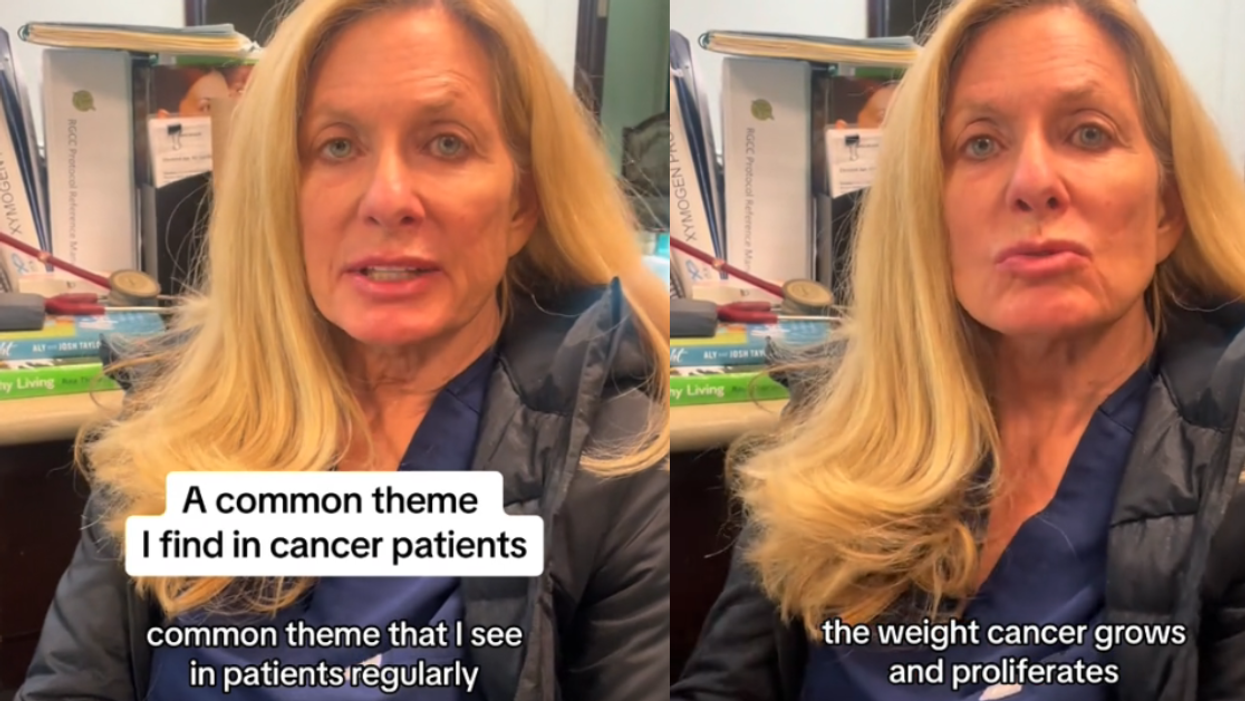





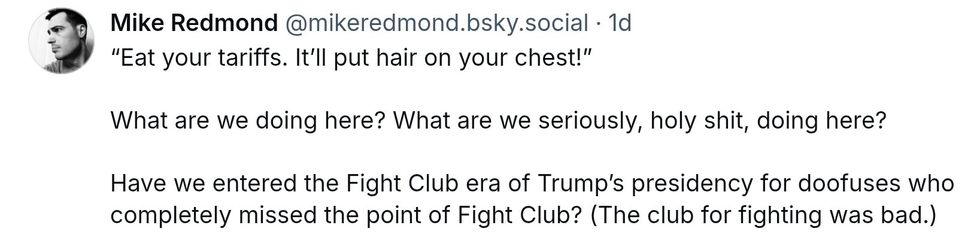 @mikeredmond/Bluesky
@mikeredmond/Bluesky

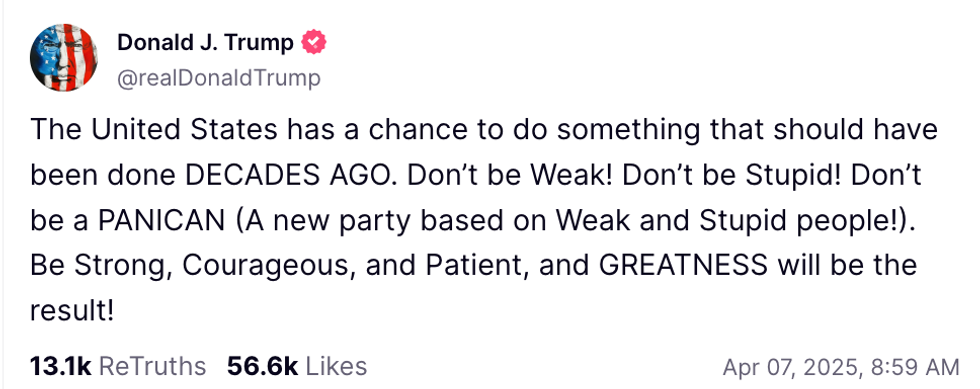 @realDonaldTrump/Truth Social
@realDonaldTrump/Truth Social