Sarah Smith battled deadly sepsis alongside her newborn baby. Now, she is urging other expectant mothers to take a $40 test that could save their little ones' lives.
Smith was delighted to discover she was expecting twins in January 2017. These would be her first children with her fiancé, Richard Townsend.
But when her 12-week scan revealed that one of the babies had acrania, a rare congenital condition where the skull does not form properly, the prognosis was so grave that she made the heartbreaking decision to terminate the pregnancy.
The twins were identical and sharing a placenta, and so the couple were told by medics that, because one baby had acrania so severely, it was highly likely had the pregnancy continued, Sarah would have miscarried at a later date or given birth to two stillborn babies.
“It was a horrible situation to be in, to be faced with having to make that decision," she said.
“But I knew before our scan that something was wrong. I could just sense it."
Four months later, it seemed there was a light at the end of the tunnel when she discovered she was expecting again, this time with a little boy.

But hours after he was born in April 2018, her son Joshua became very unwell with group B strep (GBS) meningitis, as well as sepsis, a potentially fatal illness caused by the body's response to infection. Smith was also diagnosed with it.
Smith was petrified she would lose another child. But thankfully, they both pulled through.
Now, she is determined to raise awareness of GBS, a common bacteria which can be passed to babies during labour and trigger a life-threatening infection.

The NHS does not routinely offer testing for GBS, but DIY kits can be ordered from around $40.
“Joshua was so poorly that we genuinely thought he was going to die," Smith said.
“I asked the doctors, 'Is my baby going to be okay?' and they said, 'I can't tell you that at the moment, he's very sick and we're doing what we can.'"
“We hadn't named him at that point, and I kept thinking, 'I can't let my baby pass away without a name.' Joshua wasn't even a name we discussed – I just blurted it out. For some reason, it felt right."

“Thankfully he and I are both okay, but if I'd known I could have paid £35 to take a test and save going through all of this, I absolutely would have done. It's a small price to pay for peace of mind and I really want other parents to be aware," Smith continued.
Smith's road to motherhood has been paved with difficulty. She was first diagnosed with endometriosis in 2015, and she wondered if her fertility would be affected.
Thankfully, after surgery, doctors reassured her she should be able to conceive naturally.
Her first pregnancy was a sigh of relief at first.
“Doctors initially thought I might be in pain because the pregnancy was ectopic, which is where a fertilized egg implants itself out the womb," she explained.
“But they did a scan and it turned out it wasn't ectopic at all – I was having twins. Looking back, they think the pain may have just been my body getting used to the flood of hormones."

Smith was excited for her following scans. This time, though, it revealed that one of the babies had acrania and would be unlikely to survive outside of the womb.
“The baby with acrania wouldn't have made it, but the complication was that they were twins," she said.

“There were no statistics available to us about the survival rate for the twin who looked as if they may be okay. We talked things through with the doctors, about how we could try this and that," she continued.
“In the end, we had to go with our gut. We could have ended up with two stillborn babies, a late miscarriage or one stillborn and one severely disabled baby."
“And even if the other baby had been okay, I'd have had to give birth to the one that wasn't. All of the options were difficult. I was a mess."

Smith decided to terminate the pregnancy at 13 weeks.
“Once I made my mind up, I had five days to wait for the procedure. They were the longest five days of my life. Suddenly, everywhere I looked, everyone had babies," she continued.
“The longer you wait, doubts creep in – but deep down, Richard and I both knew the babies wouldn't be okay if I continued with the pregnancy."
Four months later, Smith was pregnant again, and although this time she felt far less physically unwell, psychologically, she struggled.
“I wanted to be pregnant and I wanted a baby – but the ones I'd lost, not a new one," she added.
In a bittersweet twist of fate, her 12-week scan fell on what would have been her twins' due date, 29 September 2017.

“I was thinking, 'Is this fate telling me it'll go wrong again?' I cried before they even got the scanning equipment out," she continued.
“This time, though, everything was fine. After that, I was less anxious, but still not convinced it would be okay."
“I kept thinking, 'Just because I'm pregnant, it doesn't mean I'm having a baby. I wasn't going to be happy until he was here."

Smith went into labour in the early hours of 11 April, 2018.
However, things progressed slowly.
“By then, the baby began to get distressed, and his heart rate was dropping, so medics began to talk about a caesarean section," she recalled.
“I was taken down to theatre, and I heard someone mention a forceps delivery. I said I wanted to try that first, and thankfully they managed to get Joshua out that way."

“As he was delivered, though, I began feeling very shaky and sweaty. I was cold, but my temperature was spiking," she continued.
“I felt so weird that I couldn't even hold Joshua. Looking back, we now know that was the first symptoms of postpartum sepsis."
From there, Smith was taken to the postnatal ward to recover.
There, she became concerned when she noticed Joshua was restless, and would not stop grunting.

Then, when he was just 18 hours old, he had a seizure whilst his dad was giving him a bottle.
“It was terrifying. I pushed a button for a nurse, who came running in. In the hour that followed, he had five more seizures," Smith recalled.
“It almost looked as if he was choking. He was going blue around the mouth and medics were rushing round, attaching him to wires and putting a ventilator tube in his mouth. It was like something you see on Holby City. It's scary enough on TV, but even worse in real life. It really looked as if Joshua was going to die."
Joshua was sedated to stop his seizures and placed on a ventilator to aid his breathing.
Once he was stabilized, he was transferred to St Peter's Hospital, for more specialist care.
Smith was so unwell she could not travel with him.

“That was horrid. I wanted to be with him and when they told me they were transferring him, I took my cannula out and tried to pack my bag – but my mum and midwife said they thought I was too ill to go, and they were right," she recalled.
“I slept for a couple of hours and they brought Joshua to see me before they transferred him. At that point I couldn't stand up. I was sweating, shivering and really weak."
Medics at St Peter's suspected a GBS infection, and so Smith was swabbed to check for the bacteria.

The results came back positive, meaning they could determine that GBS bacteria had been passed to Joshua during labour, which had triggered an infection and led to sepsis.
A lumbar puncture confirmed Joshua also had meningitis.
According to the charity Group Strep B Support, testing positive for the bacteria during pregnancy is not necessarily dangerous, and those to test positive should be offered antibiotics during labour. However, in Smith's case, as she did not know she had the bacteria, she did not have antibiotics.

Symptoms of GBS infections include grunting, uncontrollable crying, not feeding well, temperature spikes, skin blotching, low blood pressure, low blood sugar, and abnormal heart rate or breathing.
Smith was also diagnosed with sepsis, and began a course of antibiotics.
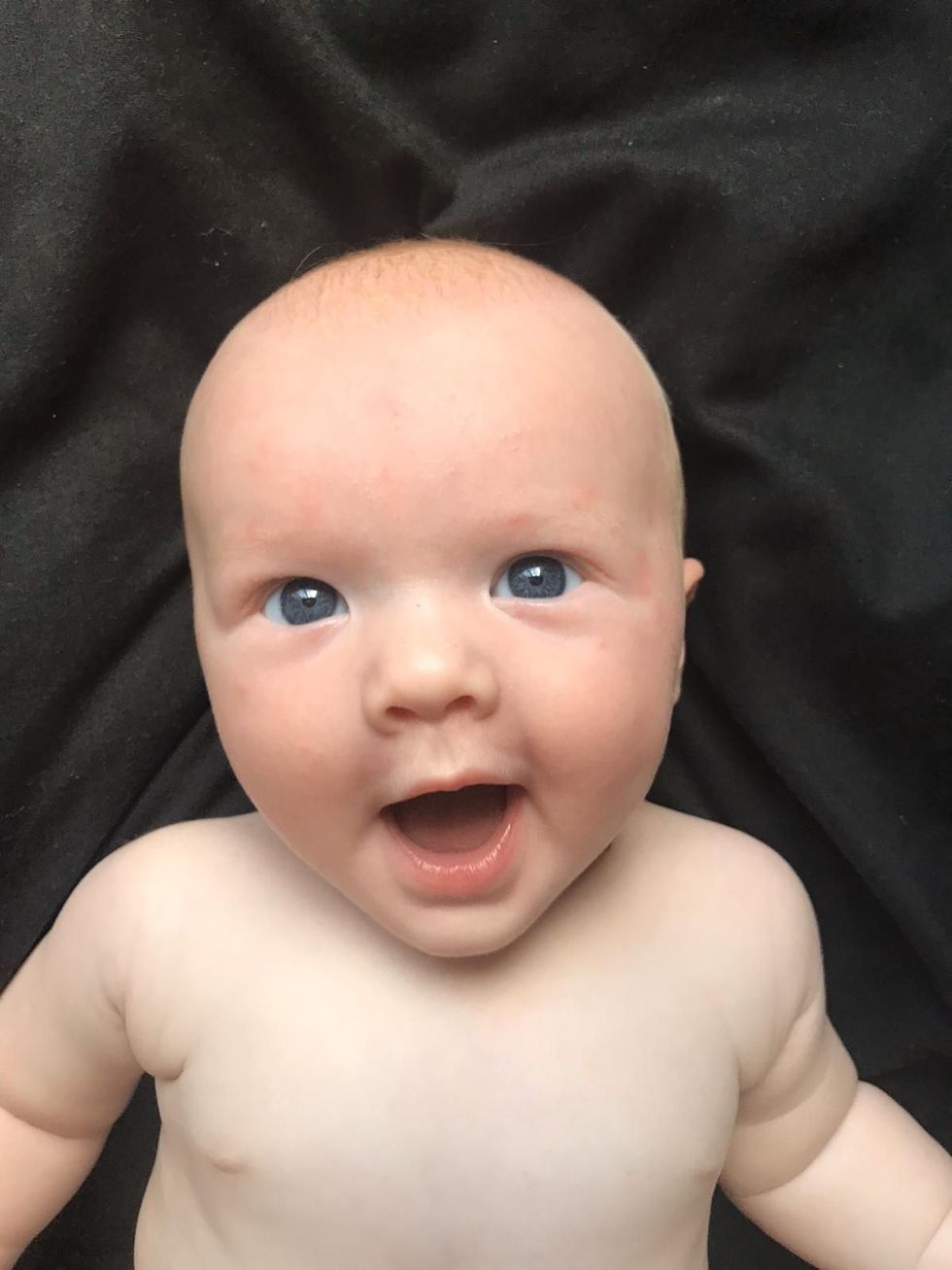
“He was born weighing 8lb 2oz, so he wasn't exactly small, but in the incubator, surrounded by all these wires and equipment, he looked tiny," she recalled.
Describing the days that followed as a “blur," Smith was discharged on April 17th, and Joshua was transferred back to Frimley Park that same day.
Though going home without her baby was difficult, the baby began responding to antibiotics and went from strength to strength.

At 15 days old, he was finally allowed home to join his parents.
“We didn't know what to do when we finally got him home. We just put him into a carry cot and stared at him," she said.
Then, when Joshua was six weeks old, Richard proposed to Smith.
“He was saying that he had put Joshua's Babygro on the wrong way round and was asking me to help," she said.
"I was getting really stressed as I'd just sat down after being on my feet all day, but when I took the Babygro off, Joshua had a little vest on saying, 'I want us to have the same surname. Will you marry Daddy?'"
“Of course, I said yes. We'd never really planned to get married but going through what we did made us realize how precious life is."
Bride-to-be Smith was planning to marry Richard in June in The Secret Walled Garden in Wasing Park, Reading, but her special day has been postponed.
Now, she is working hard to raise awareness of GBS infections.
She has successfully campaigned at her local hospital for informational leaflets to be given out as standard at antenatal appointments and is also urging mums-to-be to consider taking a private or at-home test.
“It's so important that parents know about this," Smith said. “It is just £35 but it could literally save a life."

“This case is a terrible insight into how families' lives can be almost destroyed by a GBS infection, especially since most GBS infections in newborn babies can be easily prevented," Jane Plumb MBE, Chief Executive and founder of Group B Strep Support, said.
“Testing pregnant women can save little lives and we want to see routine testing of pregnant women for GBS. Pregnant women can take this simple, safe test between 35 and 37 weeks."
“We are calling on the NHS to provide all pregnant women with information on GBS and make testing available to them. We do not want to see other families suffering as the Smiths have."
For information, visit gbss.org.uk






 Judge Judy Eye Roll GIF
Judge Judy Eye Roll GIF





 @elonmusk/X
@elonmusk/X

 Loop Home GIF by Homepoet.de
Loop Home GIF by Homepoet.de Solar Energy GIF by Nexamp
Solar Energy GIF by Nexamp
 Shave Shaving GIF by Shawn Mendes
Shave Shaving GIF by Shawn Mendes The Sandlot Wow GIF
The Sandlot Wow GIF