Any public health official interested in resolving North America’s opioid crisis should be looking towards national legalization of medical marijuana. That’s the conclusion of two new studies recently published in JAMA Internal Medicine, an American Medical Association journal.
“In this time when we are so concerned — rightly so — about opiate misuse and abuse and the mortality that’s occurring, we need to be clear-eyed and use evidence to drive our policies,” said W. David Bradford, an economist at the University of Georgia and an author of one of the studies. “If you’re interested in giving people options for pain management that don’t bring the particular risks that opiates do, states should contemplate turning on dispensary-based cannabis policies.”
A 2014 study, also published in JAMA, came to much the same conclusion: states with legalized cannabis dispensaries had a 25% lower opioid fatality rate than state without dispensaries. But the new studies are the first long-term study, based on a five-year analysis of Medicare Part D and Medicaid prescription data. The researchers conclude that in states with legal cannabis dispensaries, doctors have been referring patients with chronic pain issues to the dispensaries rather than prescribe an opioid-based painkiller.
The dispensary angle is key here. In states where either medical or recreational marijuana use is legal but no distribution infrastructure is in place, the rates of opioid prescription fulfillments declined less dramatically, between 7 and 14%. States where dispensaries are easily accessible — broadly, states that have legalized recreational marijuana use — saw the greatest drop in opioid prescription fulfillment and opioid-related deaths.
Given opioids’ notoriously spotty pain reduction (one recent study of arthritis sufferers found opioids no better than NSAIDs at pain reduction) and their infamously addictive properties, it’s not surprising that patients would choose marijuana instead. However, due to the widespread criminalization of cannabis for decades, relatively few rigorous, long-term studies of its painkilling properties are available for doctors to review.
“I would say the evidence has been very modest up until about 10 years ago, because nobody would fund the research,” said University of Maine’s Marie Hayes. “[But] people are convinced of its safety.”
Researchers are quick to point out that cannabis can have side effects, too. Several studies have indicated a link between early marijuana use and the onset of schizophrenia, though the link seems dependent on a host of variables. And there’s always the risk of getting high, though that can be mostly avoided when the psychoactive component of marijuana, tetrahydrocannabinol or THC, is removed.
Ultimately, if both opioid and cannabis painkillers are available, patients and doctors seem to be moving away from opioids. And given the epidemic usage of opioids across North America, which reaches every strata of society, that move is a net benefit for public health.








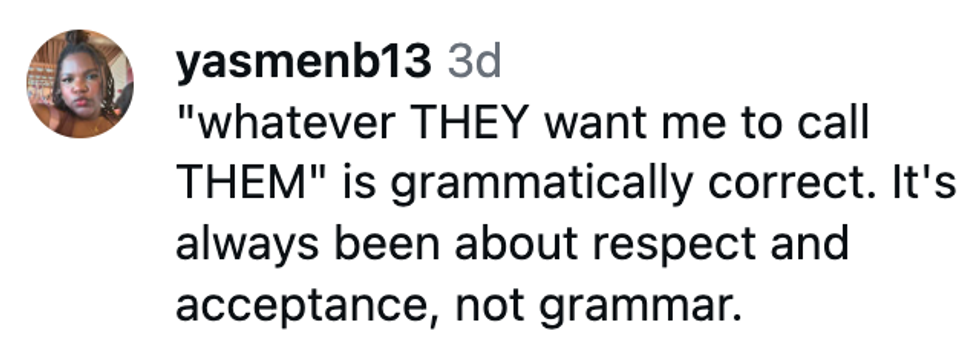
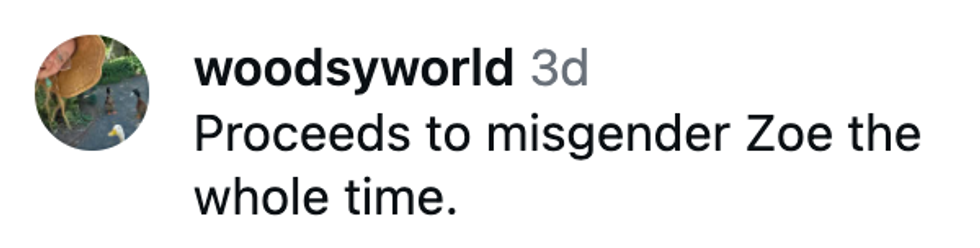
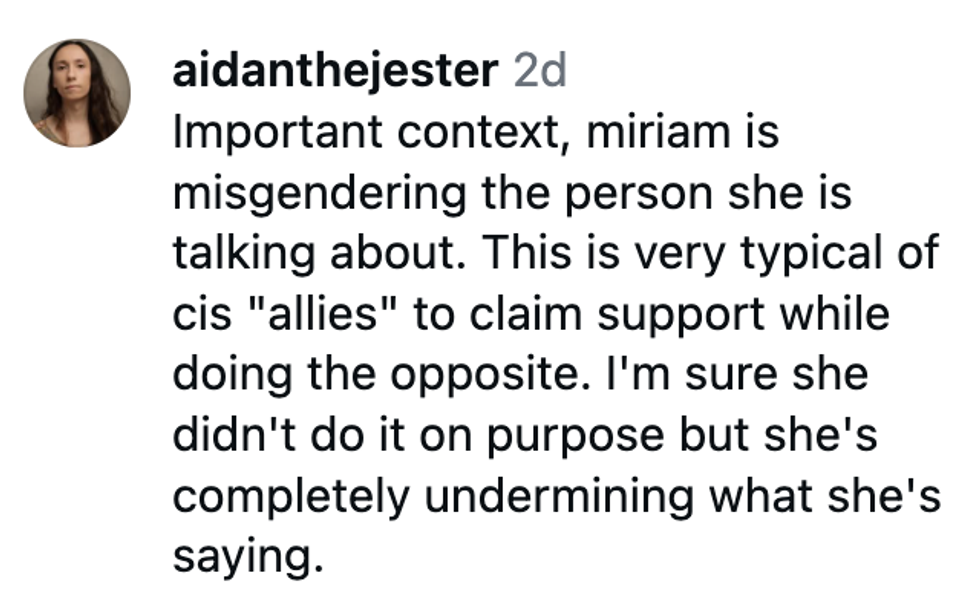







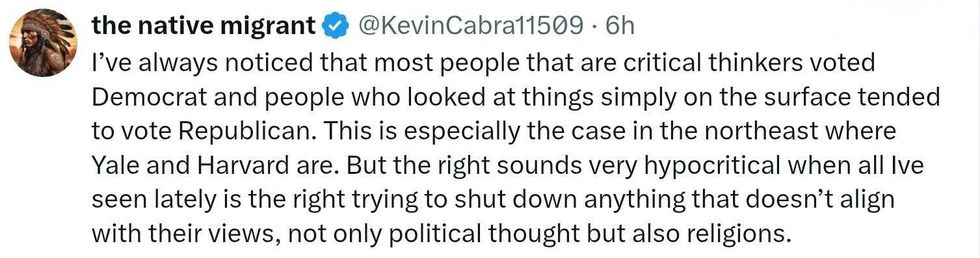 replying to @elonmusk/X
replying to @elonmusk/X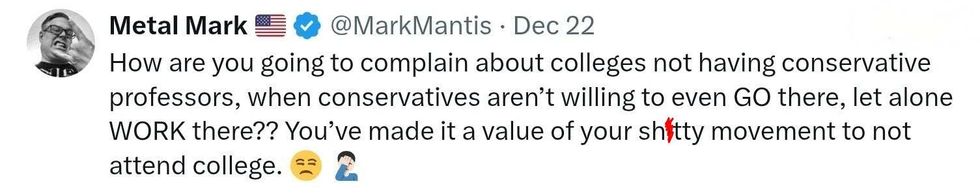 replying to @elonmusk/X
replying to @elonmusk/X replying to @elonmusk/X
replying to @elonmusk/X replying to @elonmusk/X
replying to @elonmusk/X
 Barry Manilow/Facebook
Barry Manilow/Facebook Barry Manilow/Facebook
Barry Manilow/Facebook Barry Manilow/Facebook
Barry Manilow/Facebook Barry Manilow/Facebook
Barry Manilow/Facebook Barry Manilow/Facebook
Barry Manilow/Facebook Barry Manilow/Facebook
Barry Manilow/Facebook Barry Manilow/Facebook
Barry Manilow/Facebook Barry Manilow/Facebook
Barry Manilow/Facebook Barry Manilow/Facebook
Barry Manilow/Facebook Barry Manilow/Facebook
Barry Manilow/Facebook Barry Manilow/Facebook
Barry Manilow/Facebook